 What is Plantar Heel Pain?
What is Plantar Heel Pain?
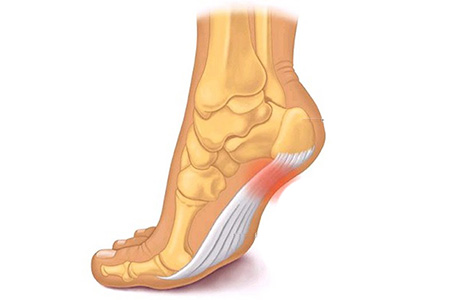
The plantar fascia is made of dense, fibrous connective tissue that will stretch very little. It acts something like a shock absorber. The fascia can become strained or torn anywhere along the course of the plantar fascia, although commonly beneath the heel, and is generally termed plantar fasciitis. This is the most common foot complaint we see and is thought to occur in 10% of the population.
Studies have shown that the fascia is not actually inflamed and therefore the term fasciitis is not strictly accurate. As a result, this can be referred to as plantar fasciosis or fasciopathy as it is more of a degenerative condition.
In reality, plantar heel pain encompasses a range of conditions which can occur separately or in combination and include:
- Thickening of the fascia (true plantar fasciitis)
- Soft tissue oedema (swelling / inflammation) above or below the fascia
- Bone marrow oedema (effectively inflammation of the bone)
- Tear
- Nerve entrapment – the small nerves beneath the heel can become irritated or entrapped causing symptoms
Calcaneal or heel spurs are often referred to in this condition. Whilst these are more common when heel pain is present, they are rarely the source of the pain and can either be part of the fascia at the insertion or sit deep to the fascia.
What causes plantar heel pain?
The most common cause of plantar heel pain is mechanical, i.e. increased stress to the fascia and includes:
- Obesity
- Poor foot function
- Unsupportive shoes
- Over activity
However, in some instances there may be rarer causes of pain and this includes:
- An underlying inflammatory condition
- Bone disease / tumours
- Infection
- Stress fracture
- Nerve entrapment in the lower back
Whilst the vast majority of cases are due to mechanical reasons, it is important to get an accurate diagnosis if symptoms are not settling with standard treatments.
Will it get worse?
Whilst plantar heel pain is a self-limiting condition (i.e. it can spontaneously go), it can last for weeks, months or years. Initially, the symptoms may be mild and only present first thing in the morning or when standing after a period of rest. However, the symptoms often become more persistent / severe until they can have a significant impact on activity levels or your day to day routine.
What are the common symptoms?
- Classic symptoms are pain first thing in the morning or on first step after rest.
- Initially, it may ease after a few steps but gradually it becomes more persistent.
- Some patients describe it like walking on hot coals or a knife sticking into the foot.
- Burning pain can be present and may represent some nerve irritation.
- Many patients experience pain around the border of the heel which can be due to walking awkwardly due to the pain beneath the heel.
How is it recognised?
- Clinical examination and a detailed history allow diagnosis.
- A detailed 3D gait analysis can help to diagnose the contributing factors.
- Many clinicians request an ultrasound scan which is helpful in identifying thickening and some tears.
- Our preference is MRI scan as it helps to differentiate between the differing pathologies that can be present and thus help us to target treatment appropriately.
What can I do to reduce the pain?
- Rest
- Ice
- Calf Stretches
- Wear supportive footwear

